Table of Contents
Introduction
What Is Covid-19 And The Main Variants In Bc
Covid-19 Symptoms In Children
Covid-19 Variants And Variants Of Concern
Covid-19 Statistics
Bc Covid-19 Data
Latest Covid-19 Information And Numbers
Ways To Keep Myself Safe
Coping With Covid-19: Mental Health And Wellness
Covid-19 Vaccines
Update On Covid-19 Vaccines
Why Should I Get Vaccinated?
Vaccine Booster
Booster Dose Timelines
Children And Covid-19 Vaccines
Vaccinating Youth Also Helps
What Are Possible Side Effects In Youth Ages 12 – 17?
If You Are Exposed To Covid-19
Covid-19 Positive Test Results
Reporting When Sick
What If Someone In My Household Or Family Tests Positive For Covid-19?
Mental Health
Trusted Sources For Information
Mental Health And Addictions
Correctional Service Canada And Covid-19
Public Health Orders
Canada’s Covid-19 Economic Response Plan
Bc’s Restart Plan
Federal Proof Of Vaccination
General Self-Isolation Supports
Food Supports
Housing Supports
Cultural & Mental Wellness Supports
Harm Reduction & Substance Use Supports
Virtual Care During Covid-19
Miscellaneous Funding Supports, Income Assistance, And Payment Deferrals
Self-Monitor & Self-Isolation Information
Crisis & Support Lines
First Nation Community Contact List
Appendix A: References
![]() Download booklet (pdf)
Download booklet (pdf)
COELS COVID-19 Resource Manual
Introduction
In March 2020, the novel Coronavirus-2019 (COVID-19) was declared a global pandemic by the World Health Organization (WHO). Pandemics can last anywhere from 12-36 months showing us the COVID-19 pandemic will be present for some time.
This manual includes resources and considerations for the continued response to COVID-19. Included in this manual is a description of what COVID-19 is, information to maintain safety, information about the COVID-19 vaccines, including booster shots, and up to date provincial protocols and guidelines. Many references were used in creating this report and are cited with the reference number in brackets (e.g., (1)); with the full reference in Appendix A.
Disclaimer: Please be aware that the information in this document is to share what has been provided at this time of the pandemic which is everchanging. If you have concerns, questions, or have allergies please speak to a healthcare provider for further information and clarification.
COELS has and will continue to adapt approaches to best support you. All the programs and services will continue following government, public health, and CSC guidelines. As those guidelines change, COELS will adapt our responses and we thank you for your patience and understanding (2).
What Is COVID-19 and the Main Variants in BC
COVID-19:
COVID-19 is a virus that affects your respiratory system causing illness to the lungs and/or other areas of your respiratory system (2). COVID-19 spreads by droplets from an infected person when they breathe, cough, sneeze, or talk near you and droplets enter your nose, throat, or eyes (6).
Some of the main COVID-19 symptoms include:
- Cough
- Fever or chills
- New loss of taste or smell
- Fatigue or weakness
- Muscle or body aches
- Shortness of breath/Difficulty breathing
- Headache
- Diarrhea, vomiting, abdominal pain (7)
- Loss of appetite
Normal body temperature
Most people have an average body temperature of about 37°C (98.6°F), measured orally (a thermometer is placed under the tongue). Your temperature may be as low as 36.3°C (97.4°F) in the morning or as high as 37.6°C (99.6°F) in the late afternoon. Your temperature may go up when you exercise, wear too many clothes, take a hot bath, or are exposed to hot weather.
Fever temperatures
A fever is a high body temperature. A temperature of up to 38.9°C (102°F) can be helpful because it helps the body fight infection. Most healthy children and adults can tolerate a fever as high as 39.4°C (103°F) to 40°C (104°F) for short periods of time without problems. Children tend to have higher fevers.
https://www.healthlinkbc.ca/illnesses-conditions/infectious-diseases/fever-or-chills-age-12-and-older
After exposure, symptoms may develop within 14 days. It is also important to note that while the symptoms are similar to a common cold, the COVID-19 virus is a potentially severe illness, particularly for people with underlying medical conditions and older adults (2).
The top five symptoms of Omicron are:
- a runny nose
- headache
- fatigue
- sneezing
- sore throat
Unlike other strains of the virus, symptoms of fever, cough and loss of smell were not as common
https://www.ctvnews.ca/health/coronavirus/what-s-it-like-having-covid-19-canadians-share-their-symptoms-amid-omicron-1.5715805
“With this Omicron variant…the incubation period, or the time between exposure and getting sick yourself and being able to pass it on to others is very small. What we’re usually seeing in five to seven days on average is now down to around two or three days.”
Shorter incubation period, more breakthrough infections in fully vaccinated: Dr. Henry
Provincial health officer Dr. Bonnie Henry says that the incubation period for the Omicron variant is a median of three days, down from an average of six days "even one month ago."
That means people who are experiencing symptoms of COVID-19 should self-isolate for one week if they are fully vaccinated, regardless of if they have confirmed the illness with a PCR test.
"If you have any symptoms of COVID-19 you must assume you have the virus and must take the appropriate measures (not to pass it on)"
COVID-19 Symptoms in Children:
Children may show COVID-19 symptoms differently than adults. For example, fatigue may show in children as poor feeding, decreased activity, or changes in behaviour.
Take your child to your nearest emergency department or call 911 if they:
- are having difficulty breathing
- have blue lips or skin, or appears very pale
- have red and/or swollen lips or tongue
- are coughing excessively, particularly with a fever
- are vomiting excessively, especially if there is blood in the vomit
- have diarrhea and vomiting, is not producing tears, and has not urinated for several hours
- have a high fever, appears very sleepy, and have not improved with acetaminophen (Tylenol) or ibuprofen (Advil).
- are under three months of age and has a fever of 38 degrees C (100.4 degrees F) or greater
- have pain or pressure in the chest that does not go away
- there is new confusion
- are unable to wake or stay awake
- have severe abdominal pain
- have a spreading rash
https://www.bccdc.ca/health-info/diseases-conditions/covid-19/about-covid-19/symptoms
COVID-19 Variants and Variants of Concern:
Like many viruses, the COVID-19 virus has changed over time and has led to new variants. There are notable ‘Variants of Concern’ (VoC) which is when the variant can spread more easily, cause more serious illness, or impact current treatments or vaccine effectiveness (10). According to the BCCDC: Five COVID-19 Variants of Concern have been detected in BC: Alpha, Beta, Gamma, Delta, and Omicron. VoC’s share genetic changes which is how they differ from one another.
https://www.bccdc.ca/health-info/diseases-conditions/covid-19/about-covid-19/variants
The best practices to maintain safety from the recent most common VoC in BC, the Omicron variant, remain the same for other existing variants. To find more information on the other known variants, please click here (10).
The Omicron variant is a new known VoC as of December 2021 has surpassed the Delta variant.
According to the BCCDC:
- Omicron has been found to spread more easily between people than previous COVID-19 variants.
- People can spread Omicron to others even if they have been vaccinated, especially when they are symptomatic.
- Omicron appears to cause less serious outcomes than other COVID-19 variants among people who have received at least 2 doses of a COVID-19 vaccine.
- Current vaccines provide good protection against severe illness and hospitalizations for Delta and Omicron
- A third vaccine dose may help provide extra protection from Omicron
- Breakthrough infections can occur in people who are fully vaccinated
- People who have had COVID-19 can get sick again from new variants.
- Getting vaccinated is important even if you have already had COVID-19.
https://www.bccdc.ca/health-info/diseases-conditions/covid-19/about-covid-19/variants
Table 1: Key Points and Maintaining Safety from the Delta Variant and VoC
| Delta Variant Facts | Maintaining Safety from Variants |
|
|
|
|
|
|
|
|
|
COVID-19 Statistics
BC COVID-19 Data
The COVID-19 Dashboard (https://www.bccdc.ca/health-info/diseases-conditions/covid-19/data#COVID-19Dashboard) shares a lot of different information, including cases, recoveries, deaths, hospitalizations, and testing. It is updated regularly and is accessible on mobiles and most browsers. (8)
Latest COVID-19 Information and Numbers
In the month of December another variant emerged and quickly became the VoC Omicron:
- The incubation period is much shorter than previous variants
- People vaccinated and unvaccinated are both catching it, the difference is the severity of symptoms
- New restrictions were put into place by the health minister to help curb this new variant
- Numbers recorded through testing were almost 5 time more than the province was seeing with the previous few variants
- Further information continues to be released and can be found on the BCCDC website
The information below is for November 2021 when the VoC was the Delta variant:
- The majority of new cases and hospitalizations continue to be among unvaccinated people.
- There is lower vaccine coverage in the Interior and Northern BC.
- The Delta variant makes up about 100% of positive tests in BC.
- The number of new COVID-19 cases is high but continues to decrease provincially; the number of new hospitalizations is generally staying the same, and the number of new deaths is relatively low and consistent.
- There are regional differences across BC in this stage of the COVID-19 pandemic. (9)
Compared with people who are fully vaccinated, unvaccinated people are:
- About 8 times more likely to have COVID-19.
- About 32 times more likely to be hospitalized because of COVID-19.
- About 20 times more likely to die from COVID-19. (9)
Ways to Keep Myself Safe
There are many ways we can keep ourselves, our families, and our communities safe and healthy. As we have seen within the best practices to ‘maintaining safety from the Delta variant’, as well as the data showing the current BC stats, we can see that a highly effective way to maintain safety is through receiving the COVID-19 vaccine. Additionally, even if we have been vaccinated (partially, fully, and booster shots), there are still health measures and protocols we can follow to help keep each other safe.
The basics still stand true as follows: IF you are feeling sick with a cough, fever, or sore throat, stay home and contact 811. You can also do the self-assessment tool online at https://bc.thrive.health/covid19/en. If it persists or gets worse, do NOT go to the hospital unless advised by medical professionals. If you have difficulty breathing, call 911 (3).
Other steps include:
- Wear a mask in indoor public spaces
- Handwash frequently with soap for as long as it takes to sing your ABC’s. twice, or to equal 20 seconds.
- Use sanitizer often.
- Practice social distancing, at least 6 feet/2 meters from others.
- Wash your masks and have several masks to be able to alternate.
- Avoid touching MEN (M-outh, E-yes, N-ose).
- Cleaning your home with household cleaning and disinfectant products (11).
- Visiting others outdoors or in small groups
Coping with COVID-19: Mental Health and Wellness
Living through a pandemic is stressful and it is normal to feel worried or anxious. FNHA (First Nations Health Authority) has produced a series of videos and fact sheets designed to help you support your mental health and wellness during this difficult time. These resources aim to explain the nature of the pandemic and the impact it might be having on your mental health. They also provide specific suggestions for dealing with the mental health and wellness issues raised by the pandemic.
The extremely contagious nature of COVID-19 means that we have to keep physically distant from others. But we can stay close emotionally. This is the time to lean on each other, and to reach out if we need support.
To view these videos, go to the FNHA website:
https://www.fnha.ca/what-we-do/communicable-disease-control/coronavirus/mental-health-and-wellness
COVID-19 Vaccines
Update on COVID-19 Vaccines
Currently, there are four authorized vaccines available in Canada, which have been through rigorous scientific review, approved, and continue to be closely monitored to ensure safety and that the benefits outweigh the risks (4). Table 2 below will help you to understand some of the similarities and differences.
Table 2: Similarities and Differences in COVID-19 Vaccines
| What is it and how does it work? | |||
| Pfizer | Moderna | AstraZeneca | Janssen (Johnson & Johnson) |
| The Pfizer vaccine is used to prevent COVID-19 by using mRNA to teach our bodies how to make a protein and build an immune response and antibodies, without the use of the live virus (2). Website link. | The Moderna vaccine is used to prevent COVID-19 by using mRNA to teach our bodies how to make a protein and build an immune response and antibodies, without the use of the live virus (3). Website link.
|
The AstraZeneca vaccine is a viral vector-based vaccines which is used to prevent COVID-19 by to teach our bodies how to make a protein and build an immune response and antibodies, without the use of the live virus (12). | The Janssen (Johnson & Johnson) vaccine is a viral vector-based vaccines which is used to prevent COVID-19 by to teach our bodies how to make a protein and build an immune response and antibodies, without the use of the live virus (13). |
| How is it given? | |||
| Pfizer | Moderna | AstraZeneca | Janssen (Johnson & Johnson) |
| Given as an injection in the muscle of the arm.
This vaccine works best by giving two doses, one dose followed by a second dose 21 days later. |
Given as an injection in the muscle of the arm.
The vaccine works best by giving two doses, one dose followed by a second dose one month later.
|
Given as an injection in the muscle of the arm.
The vaccine works best by giving two doses, one dose followed by a second dose 4 to 12 weeks later. |
Given as an injection in the muscle of the arm.
The vaccine is given in one dose. |
| How well does it work? (Efficacy) | |||
| Pfizer | Moderna | AstraZeneca | Janssen (Johnson & Johnson) |
This vaccine one week after the second dose is
|
This vaccine two weeks after the second dose is
|
This vaccine shows 74% effective in preventing COVID-19, beginning two weeks after the second dose is administered. | This vaccine shows 66% effective in preventing COVID-19, beginning two weeks after the second dose is administered. |
| Who is it for? | |||
| Pfizer | Moderna | AstraZeneca | Janssen (Johnson & Johnson) |
| People who are 5 and older. | People who are 12 and older. | People who are 18 and older. | People who are 18 and older. |
| What are the side effects? | |||
| Pfizer | Moderna | AstraZeneca | Janssen (Johnson & Johnson) |
Similarly to side effects of other vaccines, common side effects are mild to moderate and include:
As with any vaccine, there is a chance of serious side effects, but rarely occur due to the vaccine itself. This includes a possible allergic reaction. |
Similarly to the side effects of other vaccines, common side effects are mild to moderate and include:
As with any vaccine, there is a chance of serious side effects, but rarely occur due to the vaccine itself. This includes a possible allergic reaction. |
Similarly to the side effects of other vaccines, common side effects are mild to moderate and include:
As with any vaccine, there is a chance of serious side effects, but rarely occur due to the vaccine itself. This includes a possible allergic reaction. |
Similarly to the side effects of other vaccines, common side effects are mild to moderate and include:
As with any vaccine, there is a chance of serious side effects, but rarely occur due to the vaccine itself. This includes a possible allergic reaction. |
| What if I have allergies? | |||
| Pfizer | Moderna | AstraZeneca | Janssen (Johnson & Johnson) |
| Allergies for this vaccine are a potentially serious side effect, if you have known serious allergies to another vaccine, drug, or food, you should speak with your healthcare provider before receiving this vaccine (14). Website link. | Allergies for this vaccine are a potentially serious side effect, if you have known serious allergies to another vaccine, drug or food, you should speak with your healthcare provider before receiving this vaccine (4). Website link. | Allergies for this vaccine are a potentially serious side effect, if you have known serious allergies to another vaccine, drug or food, you should speak with your healthcare provider before receiving this vaccine (12). Website link. | Allergies for this vaccine are a potentially serious side effect, if you have known serious allergies to another vaccine, drug or food, you should speak with your healthcare provider before receiving this vaccine (13). Website link. |
Why Should I Get Vaccinated?
Many people have different reasons they choose to get vaccinated. Table 3 below shows some of the reasons your fellow brothers, sisters, and COELS staff chose to get vaccinated.
Table 3: Reasons for Getting Vaccinated
| Reason for Vaccination |
| Got vaccinated to protect their community from COVID-19
- To keep everyone else safe. - To protect specific people such as family, friends, coworkers, Elders, and immune compromised people. - To contribute to ending the pandemic and stop community spread. |
| Got vaccinated to protect themselves from COVID-19
- To stay safe from and prevent COVID-19 themselves. - To protect themselves from severe reactions to COVID-19 as a result of underlying health issues. |
| Got vaccinated because of public health vaccine mandates
- To follow public health mandates. - To access social activities. |
| Got vaccinated to promote safety and health (non-specific)
- To be safe. - To promote health. |
| Got vaccinated to please others or ease concerns of others
- Was persuaded by others. - Because others were getting vaccinated. |
| Other
- Felt like the right choice. - Because it was accessible and convenient. Because others accompanied them to ease fears. |
Vaccine Booster
In BC, everyone who is 18 or older will have the opportunity to have a booster dose of the COVID-19 vaccine. Booster doses will be first offered to people who are at most risk.
The benefit of a booster dose is that it helps to maintain and lengthen protection against COVID-19. By having a booster dose, you are helping to protect yourself and your community from COVID-19.
Booster doses will be Moderna or Pfizer (mRNA) vaccines, and they are interchangeable.
- Vaccines can be made by different manufacturers and vaccines that are similar but different brands can be used interchangeably “The definition of interchangeable is able to be used in place of one another” https://www.dictionary.com. There are standards in place to determine the effectiveness and safety of mixing vaccines.
- Moderna and Pfizer BioNTech are mRNA vaccines and work the same way. If you've received the first dose of one mRNA vaccine and are offered the other for your second dose, it is safe to receive it and it will offer you the same protection.
- There are multiple clinical trials and population studies of vaccine mixing taking place in countries around the world, including Canada. Results from Germany, the UK and Spain have shown the effectiveness and safety of a mixed series. We also have real-world evidence to support the process; so far over 2 million people in Canada have received a combination of COVID-19 vaccines. Canada began allowing combination COVID-19 vaccination schedules in early June and the number of COVID-19 cases and the rate of reported adverse events have continued to trend down since then.
- Completion of a two-dose series is required to be fully immunized and for long-term protection.
- A booster dose is an additional shot of vaccine that helps you maintain and lengthen your protection against severe outcomes of COVID-19. When you get a booster dose, you're helping protect you and the people around you from COVID-19. You will receive either the Moderna or Pfizer (mRNA) vaccine. These vaccines are interchangeable.
https://www2.gov.bc.ca/gov/content/covid-19/vaccine/booster
The timeline for your booster dose depends on
- Your risk level of getting COVID-19
- Your age, and
- The amount of time since your second dose
Booster Dose Timelines
Between November 2021 and January 2022, priority groups will be offered a booster shot if they are eligible. Priority groups include:
- Seniors who are 70 or older
- Indigenous people who are 18 or older
- People who live in rural and remote Indigenous communities
- People who are residents in independent living facilities and long-term home support
- Health care workers
- People who received the AstraZeneca vaccine
If you or your loved one fits into any of these categories, you can see this website for information on how to access the booster dose. Website link: https://www2.gov.bc.ca/gov/content/covid-19/vaccine/booster
Beginning in January 2022, everyone in BC who is 18 or older will be invited to have a booster shot, starting 6 to 8 months after their second dose. To have a booster shot, you must be invited and cannot drop into a clinic.
To be sure that you receive your invitation for your booster dose, your immunization record must be up to date, and you must be registered with the Get Vaccinated provincial registration system. To confirm that your immunization record is current, please follow these steps:
- If you haven't already, register with the Get Vaccinated system
- Log-in to Health Gateway to check your immunization record
- Update your immunization record if it's incorrect or if you got a dose in another province or country
Once you have received your invitation, you can use your confirmation number (which comes either in an email or text message you pick which you prefer) with it to make an appointment online or by phone. To get a dose at the same time as a family member, both people have to book a separate appointment.
Children and COVID-19 Vaccines
The COVID-19 vaccination is available for children who are five and older. Young people being vaccinated protects them and their communities from COVID-19. It is recommended that everyone who is eligible, and their communities, would benefit from having all doses of the vaccine (16).
For more information on
- How to register and book vaccine appointments for children and youth
- Information on vaccines for children who are ages 5 to 11
- Benefits of vaccination for children and adolescents
- Consent for vaccinations of young people
- And much more information on vaccinations for young people
Preparing your child for vaccine appointment:
In general, children should be informed about the vaccine close to the actual day of the vaccine. For school-age children, one day before may be appropriate.
You should encourage your child to ask any questions they may have about the vaccine. It’s important that they understand what will happen at the appointment and feel comfortable.
It may be several years since they last had a vaccine, and they may not remember it. If you have already had your COVID-19 vaccine you can share your own experience with them. Be honest.
- They may feel a pinch or poke with the needle, but it will be very quick.
- Their arm may feel heavy or sore for a few hours, but the feeling will go away.
You can also use the CARD system - Comfort, Ask, Relax, Distract to help your child find their preferred way to prepare for the vaccine.
Please see this website:
Other resources:
- Frequently asked questions about COVID-19 vaccination for five to 11 years old
- Colouring pages: COVID-19 vaccine superhero
Children in BC who are 5 to 11 years of age will be offered a Pfizer-BioNTech (CormirnatyTM) mRNA vaccine made for children their age. Health Canada approved this vaccine for children aged 5 to 11 on November 19, 2021.
The vaccine:
- Works and is safe.
- Is specially made for children.
- Was tested in children 5 to 11 years of age.
- Is a smaller dose than the vaccine given to those 12 years of age and older.
Children aged 5-11 will be offered two doses about 8 weeks apart. This includes children who have weakened immune systems. Although adults and teens with weakened immune systems need a 3rd dose to create more antibodies to better protect them from COVID-19, younger children seem to respond well to a two-dose series. A booster dose for this age group is not yet recommended.
https://immunizebc.ca/COVID-19-vaccines-FAQ-5-to-11
Youth 12 to 17 years of age will be offered either the Pfizer-BioNTech (Comirnaty™) or Moderna (Spikevax™) COVID-19 vaccine. Both of these vaccines have been approved by Health Canada for this age group. The vaccines are safe for youth, and they work.
Vaccinating youth is the best way to protect them from getting sick with COVID-19. COVID-19 tends to cause milder illness in youth compared to adults. However, it can make youth very sick, can cause them to be hospitalized, and in rare cases, can cause death.
Vaccinating youth also helps:
- Protect family members, including siblings who are too young to get vaccinated and family members who may be at increased risk of getting very sick if infected.
- Reduce the spread of the virus in the community. This helps protect people who are most at risk of getting really sick from COVID-19, including the elderly and people who are immunocompromised (have a weakened immune system, which means their body can’t fight off diseases like COVID-19 as well as people with a fully functioning immune system).
- Reduce the risk of new variants of concern emerging. We don’t know if there will eventually be a variant of concern that causes more serious illness in children and youth.
- Give youth an added layer of protection in school or while participating in sports, playdates, and other group activities.
What are possible side effects in youth ages 12 – 17?
- The most common side effects reported by youth are pain where the vaccine was given, tiredness, headache, chills, and muscle aches.
- Other common side effects of COVID-19 vaccines may include redness, soreness, swelling where the vaccine was given, joint pain, and mild fever.
- 9% of people who received the mRNA vaccines did not report any serious side effects.
- In very rare cases, myocarditis (inflammation of the heart) and pericarditis (inflammation of the outer lining of the heart) can occur. Most people recover quickly. The risk of heart complications, including myocarditis, is much greater after COVID-19 infection than after vaccination.
- A severe allergic reaction (called anaphylaxis) can happen after any vaccine, including COVID-19 vaccines, but this is rare and happens in about 1 in a million people. Should this reaction occur, healthcare providers are prepared to treat it.
https://immunizebc.ca/COVID-19-vaccination-youth-12-17-years-old
Proof of Vaccination and the BC Vaccine Card
In order to access many events, services, and businesses, we are required to show a proof of vaccination. Here are the steps to get your proof of vaccination and the BC Vaccine Card, which is also sometimes called a “QR code” (17).
A QR code is a machine-readable code consisting of an array of black and white squares, typically used for storing URLs or other information for reading by the camera on a smartphone. A QR code is a type of barcode that can hold more information than the familiar kind scanned at checkouts around the country. The “QR” stands for “quick response,” a reference to the speed at which the large amounts of information they contain can be decoded by scanners.
Step 1: Log in
To log in securely, you need to provide your:
- Date of birth
- Personal Health Number (PHN)
- Date you got dose 1 or dose 2
If you already have a Health Gateway account, log in with your BC Services Card App.
Step 2: Save or print
Once logged in, you have 3 options:
- Select "Save a copy" and save it to your phone’s photo album or computer folder
- Save a screenshot to your device
- Print a copy on paper
- It is requested that you have a digital copy on your phone. If you have circumstances/conditions, then it is important you carry a printed copy
- When you print this, you need to make sure that your QR Code is clear as it will be scanned to confirm vaccination
Step 3: Show your card
Have your card ready when entering a business. They'll look at your vaccine card and also check your government ID
Image 1: What the BC Vaccine Card looks like
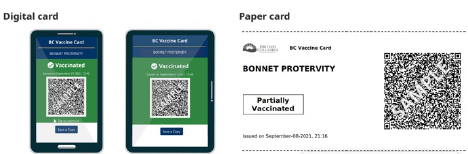
Retrieved from the Gov BC website.
If you are Exposed to COVID-19
This section shares information on what happens if you or a family get COVID-19 or are exposed to someone with COVID-19.
COVID-19 Positive Test Results
If you receive a positive COVID-19 test result, it is important to stay calm and to know that you will have a lot of support from COELS, CSC and through Public Health (2).
COELS, CSC and Public Health will work together to ensure that you are safe as well as ensure the safety of everyone else at the Healing Lodges. The following steps will generally be followed:
- Brother or Sister tests positive –Staff will follow the isolation protocols and procedures,
The Brother or Sister will immediately self-isolate in their room.
b. Staff will notify Admin, the CEO, Director of Operations, House Manager.
c. Ensuring that food is brought to the Brother’s or Sister’s room.
d. Posting a sign on the closest bathroom for use ONLY by the Brother or Sister that tested positive.
e. Practicing Universal Precautions while serving or interacting with the Brother or Sister. - CSC and Public Health will determine if the Brother and Sister are to self-isolate.
- Public Health will issue a letter directing the person testing positive for COVID-19 to self-isolate.
- CSC will identify where the Brother or Sister will self-isolate, Brothers will be moved to another facility such as a trailer in North Vancouver, Tim’s Manor and/or other locations.
- Sisters who are homeless, will be placed at a COVID-19 hotel and other community supports.
- Public Health will inform Brother and Sister when they no longer have to self-isolate.
- Brother or Sister will move back into the Healing Lodges once their self-isolation is completed, generally from 10-14 days (2).
- self-isolate (for at least five days from the first day you had symptoms if you are fully vaccinated, or at least 10 days if you are not). https://www.fnha.ca/what-we-do/communicable-disease-control/coronavirus/covid-19-rapid-testing/
COELS is not able to provide a safe space at this time for individuals to self-isolate in the Healing Lodges. Your cooperation and understanding as you go through this incident will ensure that you are safe and that those that live and work within the Healing Lodges and by extension their families are safe as well (2).
Reporting when sick
If you have been exposed to someone with COVID-19, you may need to quarantine. It is important to quarantine if:
- You lived with them
- You have been physically close to them, such as caring for them or being intimate
- You have been exposed to their bodily fluids, such as their coughing or sneezing
If you or a family member is sick with COVID-19 or has been exposed to COVID-19, please contact, and follow instructions from your local public health authority about quarantining and when to return to work (18).
Yes, you still need to self-isolate if you are tested for COVID-19 and the result is negative for 10 days from the last time you were exposed to someone who has COVID-19, unless you are fully vaccinated. If you are fully vaccinated, you should stay home until you feel well enough to return to normal activities.
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/self-isolation/close-contacts
- If you have mild symptoms and are fully vaccinated, you do not need a test. Stay home and away from others for five days, and then you can go about your business as long as you're feeling better, and you no longer have a fever or symptoms.
- If you do not have symptoms of COVID-19, you do not need a test.
- If you feel unwell and are unsure about your symptoms, contact your health care provider or call 8-1-1
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/testing/when-to-get-a-covid-test/
What if someone in my household or family tests positive for COVID-19?
For information on how to care for someone at home who has been or may have been exposed to COVID-19, you can see this website. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/how-care-someone-covid-19-home.html
This page linked above also includes information on
- Supplies needed
- How to provide care as safely as possible
- How to protect yourself and others who live together
- How to clean and disinfect
- How to monitor for symptoms and seek medical care if needed
- When, how, and how long to quarantine for
How to test using a BTNX COVID-19 Rapid Antigen Test
You will need
- 1x sterile swab
- 1x test tube
- Plastic vial with buffer liquid
- Test tube rack or a small glass
- 1x test device
- Timer and garbage can
- Blow your nose and discard the tissue
- Do not use this test if you have a nose bleed
- Wash your hands with soap
- Gather all testing equipment
Step 2 - Get the tube ready
- Twist the top off the buffer liquid vial.
- Squeeze all the buffer liquid into the test tube.
- Place the filled test tube in the test tube holder or a clean glass or cup.
Step 3 - Collect the sample
- Remove the swab from the packaging. Touch only the plastic handle.
- Tilt your head back.
- Insert the cotton end of the swab straight back(not up) into one nostril for 2.5 cm or when you meet resistance
- Turn the swab against the inside of your nose for 5 seconds.
- Press the side of your nose with your finger to trap the swab. Rotate the swab for 5 seconds
- Repeat same steps in your other nostril.
- Do not use the swab for testing if there is any blood on it. Blow your nose and use a clean swab. If you have had a nose bleed wait 24 hours before testing.
Step 4 - Perform the test
- Gently insert the cotton end of the swab into the test tube:
- Swirl the swab gently in the liquid and squeeze the swab with the sides of the tube 10-15 times.
- Place the tube in the glass or test tube rack and leave with the swab in the solution for 2 minutes.
- With the swab inside, pinch the outside of the tube with your fingers to get the remaining liquid out of the swab tip.
- Remove the swab and put in the garbage.
- Attach the nozzle to the tube.
Step 5 - Test device
- Open a test device and place it on a flat surface.
- Slowly squeeze 3 drops onto the circle on the test device.
Step 6 - Get your results and clean up
- Set a timer for 15 minutes. Readings after 20 minutes may not be accurate.
- Do not move the test device during this time.
- Check your result. Your result could be:
- Positive
- Negative
- Invalid
- Put all testing equipment in the garbage
- Wash your hands.
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/testing/rapid-antigen-testing#btnx
Long-term effects of COVID-19
We know in some cases of COVID-19 there have been very few symptoms, however this does not mean there are no potential long-term effects of COVID-19. The CDC is actively working to learn more about the whole range of short- and long-term health effects associated with COVID-19. As the pandemic unfolds, we are learning that many organs besides the lungs are affected by COVID-19 and there are many ways the infection can affect someone’s health.
According to the Merriam-Webster Dictionary “Long Haul” is defined as: “a considerable period of time: LONG RUN — usually used in the phrases for the long haul, over the long haul, and in the long haul” https://www.merriam-webster.com/dictionary/long%20haul
While most persons with COVID-19 recover and return to normal health, some patients can have symptoms that can last for weeks or even months after recovery from acute illness. Even people who are not hospitalized and who have mild illness can experience persistent or late symptoms (2).
About
You can develop post COVID-19 conditions if you had a severe case of COVID-19 and needed hospitalization, or if you had mild infection, or even no symptoms, and it can affect both children and adults.
When people still show symptoms of COVID-19 for weeks or months after their initial recovery, it’s called post COVID-19 condition. It’s also known as long COVID.
Post COVID-19 condition may occur in some people after infection. You can get post COVID-19 condition if you:
- were hospitalized or needed intensive care during recovery or
- had a mild to severe infection with symptoms or even mild infection without symptoms
Post COVID-19 condition is not COVID-19. Symptoms can be quite different from those during the initial infection. It refers to the longer-term effects some people experience after their COVID-19 illness.
Symptoms
Post COVID-19 condition can have different symptoms for different people. Some of the most common symptoms are listed in the table 4 below.
Table 4: Common Symptoms of Post COVID-19 Condition
| Most common symptoms in adults | Most common symptoms in children |
|
|
A good idea is to keep a symptom journal which can help identify patterns to symptom fluctuations over time.
Mental Health
It is normal for COVID-19 exposure or sickness to affect mental health. Talk to your health care provider if you are experiencing symptoms of anxiety, depression or PTSD related to your illness to access support.
Prevention and Treatment
The best way to prevent post COVID-19 condition is to take measures to prevent getting COVID-19. For example, being vaccinated can reduce the likelihood of you getting COVID-19. There is no treatment for post COVID-19 condition, but you can speak to your health care provider for support on how to manage symptoms.
Trusted Sources for Information
There is a lot of information that we need to know about COVID-19 and not all of it is reliable.
Some tips to best navigate the information include:
- Assess the source
- Go beyond the headlines
- Identify the author
- Check the date
- Examine the supporting evidence
- Check your assumptions and biases
- Turn to fact-checkers
For more information about navigating COVID-19 information, misinformation, and disinformation, please see this website: http://www.bccdc.ca/health-info/diseases-conditions/covid-19/covid-19-vaccine/how-to-find-trusted-information-about-vaccines
In a recent survey completed by COELS Brothers, Sisters, and staff, the top identified trusted source of COVID-19 information is from health authorities. Accessing information from your local health authority is a reliable and trusted source of relevant, and up-to-date information for your local COVID-19 information.
- For more information about COVID-19 from the Vancouver Coastal Health Authority, please see this website: http://www.vch.ca/covid-19
- For more information about COVID-19 from the First Nations Health Authority, please see this website: https://www.fnha.ca/what-we-do/communicable-disease-control/coronavirus
Mental Health and Addictions
The pandemic has resulted in many changes that may have impacted our mental health. It is important that we acknowledge and care for our mental health as we navigate the COVID-19 pandemic. You may have a lot of difficult feelings around the pandemic, including stress, uncertainty, fear, loss, and maybe even hopelessness. It is important for you to know that you are not alone.
There are many simple and accessible steps we can take, to take care of our mental health and well-being during this collective challenging time.
For available support programs through the Canadian Mental Health Association, please see this website for more information: https://cmha.bc.ca/covid-19/
For tips for taking care of yourself and additional information to get help, please see this website for more information: please click here
If you would like to speak to an experienced and culturally safe counsellor for Indigenous specific support, you can:
- Call the Hope for Wellness Help Line at 1-855-242-3310 (toll free) 24/7.
- Connect to the online Hope for Wellness chat at https://www.hopeforwellness.ca
The Hope for Wellness Help Line offers immediate mental health counselling and crisis intervention to all Indigenous peoples across Canada.
Experienced and culturally competent Help Line counsellors can help if you:
- want to talk
- are distressed
- have strong emotional reactions
- are triggered by painful memories
If asked, counsellors can also work with you to find other wellness supports that are available near you
Phone and chat counselling is available in English and French. On request, phone counselling is also available in:
- Cree
- Ojibway
- Inuktitut
The Government of Canada also has information related to mental health and addictions and COVID-19. There is information related to mental health and wellness, raising awareness, and reducing stigma as well as further resource materials https://www.sac-isc.gc.ca/eng/1576089278958/1576089333975.
Correctional Service Canada and COVID-19
For the latest updated information on COVID-19 in federal correctional institutions, see this website: https://www.canada.ca/en/correctional-service/campaigns/covid-19/latest-information.html
The website includes information on vaccines and testing for people who are incarcerated, visiting those who are incarcerated, and related information.
Corrections Service Canada has also posted the messages from the Commissioner to the inmates throughout the country. https://www.canada.ca/en/correctional-service/campaigns/covid-19/offenders-families.html
Public Health Orders
There are some provincial restrictions which are in place to help stop the spread of COVID-19. Some regional restrictions continue to be in place for health authorities with lower vaccination rates. For more information on these regional restrictions, please check out the following link:
https://www2.gov.bc.ca/gov/content/covid-19/info/restrictions
The website also has information on:
- Requirement for mask-wearing
- Requirements for gathering and events
- Requirements for restaurants, pubs, and bars, and
- Guidance on visiting long-term care or senior’s assisted living facilities
Canada’s COVID-19 Economic Response Plan
CERB and Canada Recovery Benefit (CRB) have now closed. There are other COVID-19 supports which you may be eligible for here: https://www.canada.ca/en/department-finance/economic-response-plan.html
They include, as of November 2021:
Table 5: COVID-19 Financial Support
| Support | Details |
| Employment Insurance (EI) |
|
| The new Canada Worker Lockdown Benefit |
|
| Canada Recovery Sickness Benefit |
|
| Canada Recovery Caregiving Benefit |
|
Sick Days
As of January 1, 2022, most workers in BC will not have to decide between losing wages or having to work when sick. BC is planning to implement permanent paid sick leave which comes into effect with 5 paid sick days each year. Both full- and part-time employees are eligible for this benefit (22).
BC’s Restart Plan
The government of BC has a 4-step process planned to gradually reduce COVID-19 restrictions. In order to move from each step to the next, our communities need fewer COVID-19 cases, increased vaccinations, fewer hospitalizations, and fewer COVID-19 related deaths.
Information on the 4 steps for offices and workplaces, travel and sports and recreation are in the table below. See this website for more details and information on the restart plan for personal gatherings, organized gatherings, and businesses: https://www2.gov.bc.ca/gov/content/covid-19/info/restart
Table 6: Government of BC’s Restart Plan (retrieved from BC Government Website)
| Offices and Workplaces | Travel | Sports and Recreation | |
| Step 1: | Start a gradual return to workplaces
Employers must continue to have a COVID-19 Safety Plan and daily health check in place |
Recreational travel within your travel region allowed
Non-essential travel between travel regions continues to be restricted |
Indoor low intensity group exercise allowed with limited capacity
Outdoor games and practices for both adults and youth group/team sports allowed No spectators at any indoor or outdoor sport activities |
| Step 2: | Continued return to the workplace
Small, in-person meetings allowed Employers must continue to have a COVID-19 Safety Plan and daily health check in place |
Recreational travel within B.C. allowed
BC Transit and BC Ferries offers increased service as needed |
Indoor high and low intensity group exercise allowed with reduced capacity
Indoor and outdoor games and practices for both adults and youth group/team sports allowed Outdoor spectators up to 50 allowed, no spectators at any indoor sport activities |
| Step 3: [CURRENT STAGE] | Continued return to the workplace
Seminars and bigger meetings allowed Additional safety precautions required in higher risk workplaces. |
Canada-wide travel, check provincial/territorial restrictions
International travel, if fully vaccinated and in line with federal travel guidance Federal proof of vaccination is required for some domestic and international travel. The government of British Columbia outlines what is needed for travelling within Canada and internationally. https://www2.gov.bc.ca/gov/content/covid-19/travel/current Returning to Canada When you return to Canada, you must use ArriveCAN to submit your travel and health details in the 72 hours before your arrival back in the country. Travellers arriving from all countries except the United States must take a COVID-19 test on arrival in Canada and self-isolate until they receive a negative test result. |
All indoor fitness classes allowed, normal capacity
Gyms and recreation facilities, normal capacity Outdoor spectators 5,000 people or 50% capacity, whichever is greater Indoor spectators, normal capacity Proof of vaccination is required for spectators and adult participants at indoor and outdoor sporting events. |
| Step 4: | Businesses will continue to follow communicable disease prevention guidance | Canada-wide recreational travel
International travel, in line with federal travel guidance |
Return to normal sport competitions when following communicable disease prevention guidance
Increased outdoor and indoor spectators |
As COVID-19 continues to change so will the restrictions. There will be provincial and regional restrictions in place by the health minister which are there to help stop the spread of COVID-19. Sometimes there will be time constraints placed on the restrictions, orders, and regulations. The government of British Columbia website is regularly updated with all restrictions, orders, and regulations.
https://www2.gov.bc.ca/gov/content/covid-19/info/response
Federal proof of vaccination
You will get your proof of vaccination online for British Columbia using Health Gateway.
Proof of vaccination is free to get. If someone is asking you to pay for these documents, it's a scam.
Step 1: Log in securely at https://www.healthgateway.gov.bc.ca/vaccinecard
Enter your information:
- Date of birth
- Personal Health Number (PHN)
- The date you got dose 1 or dose 2
You can also log in with your BC Services Card.
Step 2: Save or print a copy
- Click the Save as button
- Select Image (BC proof) or PDF (federal proof)
- Save a copy, take a screenshot, or print a paper copy
Note: If you're travelling, keep a paper copy of your federal proof of vaccination as a back-up.
Step 3: Show your proof of vaccination
Have your proof of vaccination and government ID ready when entering a place that requires proof or when travelling.
Feel safe knowing that everyone around you is vaccinated.
https://www2.gov.bc.ca/gov/content/covid-19/vaccine/proof#card
*Courtesy of Aboriginal Health and Vancouver Coastal Health
COVID supports in VCH region
Please note: services may be listed under multiple headings to help with navigation
Other supports may be available to Patients through VCH and the COVID Outreach Team
General self-isolation supports
| Support & contact information | Brief Description & Eligibility |
| First Nations Health Authority (FNHA)
Health Benefits Self-Isolation Support team 1-888-305-1505 |
self-isolation support (travel, meals, accommodation)
8:30am-4:30pm 7d/wk *Status First Nations |
| Individual Nations
Community level support |
community-level supports may be available.
*Status First Nations |
Food Supports
| Support & contact information | Brief Description & Eligibility |
| Pacific Association of First Nations Women
Good Food Box & emergency housing subsidies - Online application: https://tinyurl.com/reachinghomegfb OR |
Food delivery (e.g. grocery store food items, prepared meals, fresh fruit and vegetables)
Will be placed on a wait list, with follow up if support becomes available *Lower mainland residents only. Open to Indigenous women and children |
| First Nations Health Authority (FNHA)
Health Benefits Isolation Support team 1-888-305-1505 |
self-isolation support (travel, meals, accommodation)
8:30am-4:30pm 7d/wk *only Status First Nations who have qualified for self-isolation support (see above) |
| Support Network for Indigenous Women & Women of Colour
|
Food delivery Support for Women in isolation |
| Vancouver: https://vancouver.ca/people-programs/covid-19-coronavirus-help-get-and-give-food.aspx
Vancouver, Richmond, North Shore: http://www.vch.ca/public-health/nutrition/food-asset-map |
|
Housing Supports
| Support & contact information | Brief Description & Eligibility |
| Pacific Association of First Nations Women
emergency housing subsidies - Online application: https://tinyurl.com/reachinghomegfb OR |
Will be placed on a wait list, with follow up if support becomes available
*Lower mainland residents only. Open to Indigenous women and children |
Cultural & Mental Wellness Supports
| Support & contact information | Brief Description & Eligibility |
| Tsow-tun-le lum:
1-888-403-3123 (toll-free) Or contact via facebook messaging |
Cultural support & counselling by phone or video |
| Indian Residential School Survivors Society
Resolution Health Support Workers Executive Director: Angela White |
Emotional support services during isolation
*Urban, Indigenous, and directly affected by COVID |
| Indian Residential School Survivors Society
Virtual cultural support |
Traditional healing and medicines by phone or video
*Urban, Indigenous, and directly affected by COVID |
| Pacific Association of First Nations Women | by phone or video (zoom)
*Indigenous folks of all genders and ages |
| Pacific Association of First Nations Women
COVID-19 Counselling |
Counselling by phone or video (zoom)
*Indigenous folks of all genders and ages |
| VCH Aboriginal Health
Virtual cultural support 1-877-875-1131 (toll-free) |
Cultural and emotional support by phone or video provided by VCH Elders/Knowledge Keepers
*Indigenous folks of all genders and ages in need of additional support |
| FNHA | Referral-based (no-cost) service
Substance Use and Addictions Medicine: Monday to Friday 9:30am-5:30pm Psychiatry: Monday to Friday 10am-3pm. *Available to all BC First Nations people and their families, even if family members are not Indigenous |
| Spirit of the Children Society
Cultural teaching (virtual) 604-524-9113 |
Virtual cultural teachings (zoom)
Mondays 4-5pm *Youth aged 7-18 |
| Broadway Youth Resource Centre
Queer, Trans, & Two-Spirit zoom social Lindsay McKinnon 778-877-0993 |
Weekly zoom socials
*Youth aged 14-24 who identify as queer, trans, or two-spirit |
| QMUNITY
Youth drop-in |
Virtual drop-in (zoom) Mondays 4-5pm
*queer youth aged 14-25 |
| Spirit of the Children Society
604-524-9113 |
Virtual youth group (zoom) Wednesdays 4-5pm
*Youth aged 13-18 |
| Foundry
Virtual counselling 1-833-308-6379 online@foundrybc.ca OR |
Free virtual counselling (phone or video)
1:15-9pm Monday-Friday *Youth aged 12-24 |
| WAVAW
604-255-6344
|
Phone counselling and support groups using a holistic approach utilizing traditional teachings and ceremonies
Also do Community referrals * Indigenous people of marginalized genders, including trans and cis women, as well as trans, non-binary, and Two Spirit people seeking health, wellness, and safety |
| WAVAW
604-255-6344
|
One-to-one counselling and support groups
*survivors of marginalized genders: cis and trans women, Two-Spirit, trans and/or non-binary people who have experienced sexual assault |
| 2 Spirits of BC | Online Talking Circle (Zoom)
Tuesdays @ 7pm *Indigenous 2-Spirits living in BC |
| Support Network for Indigenous Women & Women of Colour | Free counselling for low income, racialized women |
Links to additional mental wellness and cultural resource listings
| Link/Source | Brief Summary |
| Virtual Mental Health Supports During COVID-19 (Government of Canada) | - List of virtual mental health supports available |
| COVID-19 Mental Health and Cultural Supports (FNHA)
|
- Full list of Mental Health Support available for community members, community leaders
- List of cultural support |
| Staying Connected During the COVID-19 Pandemic (FNHA) | - Poster |
| Mental Health & Wellness Resources (FNHA) | - Links to videos, fact sheet, poster, news article |
| Database of youth support programs and services in communities across Canada
(Kids Help Phone) |
- Service locator for youth support programs and services |
Harm Reduction & Substance Use Supports
| Support & contact information | Brief Description & Eligibility |
| Western Aboriginal Harm Reduction Society OutreachWAHRS Coordinator: Tracey Draper (604) 374-3594 |
Delivery of harm reduction supplies, food, and hydration
*Indigenous folks in the DTES area |
Virtual Care during COVID-19
| Link/Source | Brief Summary |
| FNHA
1-855-344-3800 to book an appointment |
Virtual primary healthcare 8:30am-4:30pm 7d/wk
*Available to all BC First Nations people and their families, even if family members are not Indigenous |
| FNHA | Referral-based (no-cost) service
Substance Use and Addictions Medicine: Monday to Friday 9:30am-5:30pm Psychiatry: Monday to Friday 10am-3pm. *Available to all BC First Nations people and their families, even if family members are not Indigenous |
Miscellaneous Funding Supports, Income Assistance, and Payment Deferrals
| Support & contact information | Brief Description & Eligibility |
| Indian Residential School Survivors Society
Funding supports Executive Director: Angela White
|
Funding supports for every day necessities (medicine, food, etc.)
Limited funding available – have family name, contact information, number of adults/children, and summary of needs ready *Urban, Indigenous, and directly affected by COVID |
| Métis Nation BC (MNBC)
Emergency COVID supports Apply through online portal: www.mnbc.ca/covid OR contact Regional Health Coordinator: Arathy Menon 604-202-2873 (cell) |
Emergency COVID supports may be available if other resources have been exhausted via online portal application system
*MNBC (Métis) citizens |
| Métis Chartered Communities (MCC) (North Fraser & Powell River)
President, Métis Nation Powell River: Tabatha Berggren 604-223-5856 OR contact Regional Health Coordinator: Arathy Menon 604-202-2873 (cell) |
Some supports available through MCC presidents
*Self-identified Métis living in qathet Regional district (formerly Powell River Regional District); Richmond; and Vancouver |
| Province
BC Recovery Benefit Online application https://www2.gov.bc.ca/gov/content/economic-recovery/recovery-benefit |
one-time payment of up to $1,000 (families) and up to $500 (individuals)
*eligible individuals with net income up to $87,500 and eligible families with net income up to $175,000 full eligibility criteria on website |
| Government of Canada | Information on:
· Employment insurance (EI) · Canada Recovery Benefit (CRB) · Canada Recovery Sickness Benefit (CRSB) · Canada Recovery Caregiving Benefit (CRCB) · Mortgage payment deferral |
| Government of Canada | |
| BC Hydro
Customer Crisis Fund (CCF) 1-800-BC-HYDRO |
Bill deferral, payment plans, as well as crisis funding is available.
*Residential customer experiencing a temporary financial crisis |
| ICBC
Monthly payment deferral 1-800-665-6442 |
Monthly payment deferral by up to 90 days |
Self-Monitor & Self-Isolation Information
| Link/Source | Brief Summary |
| Self-isolation post COVID-19 testing (BCCDC) | - Resource on self-isolation |
| How to self-isolate - Handout (VCH) | - Hand on posters |
| Guide for Caregivers and Household Members of those with COVID-19 (VCH) | - Information for caregiver and household member living with someone self-isolating |
| How to self-isolate at home when you may have been exposed to COVID-19 and have no symptoms
(3 pager PDF)(Public Health Agency of Canada) |
- General resources
- 3-pager on self-isolation considerations |
| Be Prepared (COVID-19) (Health Canada) | - Poster on how to plan for self-isolation/self-monitor |
| Health Benefit Self-Isolation Support (FNHA) | - Available seven days a week from 8:30 a.m. to 4:30 p.m. Call 1-888-305-1505
- For eligible individual to secure self-isolation in or near community |
| Visiting the Hospital (VCH) | - Latest information on visiting a VCH hospital |
| COVID infection control - client transportation (FNHA) | - Guide on steps to support client transportation |
Crisis & Support Lines
| Support & contact information | Brief Description & Eligibility |
| Indian Residential School Survivors
24 hour Crisis Line 1-866-925-4419 |
*Available for anyone experiencing pain or distress as a result of their residential school experience |
| Kuu-Us Crisis Line
24 hour Crisis Line 1-800-588-8717 (toll-free) 250-723-2040 (youth line) 250-723-4050 (adult line) |
Indigenous and First Nations specific crisis line
BC only |
| Battered Woman's Support Services Crisis Line
1-855-687-1868 (toll-free) |
Monday-Friday 10am-5pm (Wednesday until 8pm)
· Emotional support & Safety planning · Referrals to transition houses, lawyers, medical services, community support *Services open to all women (specific supports available for immigrant and Indigenous women) |
| Kids Help Phone
1-800-668-6868 (toll-free) https://kidshelpphone.ca/ OR text 686868 (texting service) https://www.facebook.com/CrisisTextLinepoweredbyKidsHelpPhone (crisis text line via facebook messenger) |
24 hour phone service connecting kids to counsellors and crisis responders
currently available in English, French, and Arabic *Open to all children and youth |
| Suicide Crisis Line
1-800-784-2432 www.YouthInBC.com (online youth chat) |
24 hour crisis line available in over 140 languages
Online chat service: noon-1am *Open to anyone experiencing thoughts of suicide |
| Métis Crisis Line
1-833-Metis-BC (1-833-638-4722) |
24 hour phone support for immediate crisis intervention and mental wellness supports
*Self-identified Métis folks living in BC |
| Women Against Violence Against Women 24 hour Crisis and Information Line
604-255-6344
|
24 hour non-judgemental support, can provide information on available WAVAW services or referrals to other community programs/organizations
*survivors of sexualized violence |
| Trans Lifeline Hotline
1-877-330-6366 |
Peer support phone service run by trans people for trans and questioning peers
guaranteed call operators 7am-2am *those in need of someone trans to talk to |
First Nation Community Contact List
| Region | Community | Nurses |
| Central Coast
|
Heiltsuk (Bella Bella) | Mitch Savage ( CHN/Nurse Supervisor)
Phone: (250) 957-7944 |
| Central Coast
|
Kitasoo/ Xai'xais (Klemtu) | Kathryn Chapman (Nurse in Charge)
Note: Nurse in Charge changes, best to call ahead of time and confirm. Phone: (250) 839-1221 |
| Central Coast
|
Wuikinuxv (Rivers Inlet) | April Shea, (Home Care Nurse)
Phone: (250) 949-8625 ext 226/225 |
| Central Coast
|
Nuxalk (Bella Coola) | Kirsten Milton (Health Director)
Phone: (250) 799-5809
Sophie Mack (Community Health Nurse) sophie.mack@fnha.ca Phone: (250) 267-5486 |
| Central Coast/Cariboo | Ulkatcho (Anahim Lake) | |
| Sea to Sky
Southern Stl’atl’imx
|
Lil’wat | Michelle Headley (Nurse Supervisor)
Nikki Hunter( Home Care Manager) Phone: (604) 894-6656 ext.3231 |
| Sea to Sky
Southern Stl’atl’imx
|
Southern Stl’atl’imx Health Society
Four communities: N’Quatqua, Skatin, Samahquam, Xa’xtsa (Douglas/Tipella) |
Pamela Jules (Nurse Supervisor)
Phone: (604) 902 5015
|
| Sunshine Coast
(South)
|
shíshálh (Sechelt) | Nick Gaskin (Health Director)
Phone: 604-399-8717
Tamara Guretzki (Home Care Nurse)
Shiloh Joe, (Division Manager) Phone: (604) 885-9404 |
| Sunshine Coast
(North)
|
Tla'amin (Sliammon/Powell River) | Melinda Hasselback (Chronic Disease Nurse)
Phone: 604-483-3009 |
| Lower Mainland
|
Musqueam | Crystal Point (Community Health Nurse)
Phone: (604) 269-3313 |
| Lower Mainland
|
Squamish | Samantha Clarke (Home Care Manager)
Phone: (604) 318-4418 |
| Lower Mainland
|
Tsleil-Waututh Nation | Sibylle Tinsel (Community Health Nurse)
Phone: (604) 353-5314 |
The above information is courtesy of Aboriginal Health and Vancouver Coastal Health
Appendix A: References
- Brothers-and-Sisters-COVID19-Manual-Workbook-Revised-2020:
https://www.circleofeagles.com/wp-content/uploads/2021/09/Brothers-and-Sisters-COVID19-Manual-Workbook-Revised-2020-72dpi.pdf - COELS-Coronavirus-Pandemic-Response-Planning-Guide-2020:
https://www.circleofeagles.com/wp-content/uploads/2021/09/COELS-Coronavirus-Pandemic-Response-Planning-Guide-2020-72dpi.pdf - Brothers-and-Sisters-Manual-for-COVID-19-Vaccines-Basic-Information:
https://www.circleofeagles.com/wp-content/uploads/2021/09/Brothers-and-Sisters-Manual-for-COVID-19-Vaccines-Basic-Information-72dpi.pdf - BCCDC > How it Spreads:
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/aboutcovid-19/how-it-spreads - Government of Canada > Coronavirus disease (COVID-19): Symptoms and Treatment:
https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/symptoms.html - BCCDC > BC COVID-19 Data:
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/data#COVID-19Dashboard - BCCDC > BCCDC COVID Data Summary: 18 November 2021:
http://www.bccdc.ca/Health-Info-Site/Documents/COVID_sitrep/2021-11-18-Data_Summary.pdf - BCCDC > COVID-19 Variants:
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/about-covid-19/variants - BCCDC > Cleaning and Disinfecting:
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/prevention-risks/cleaning-and-disinfecting - Government of Canada > AstraZeneca Vaxzevria COVID-19 Vaccine:
https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/astrazeneca.html - Government of Canada > Janssen (Johnson & Johnson) COVID-19 Vaccine:
https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/janssen.html - Government of Canada > Pfizer-BioNTech COVID-19 Vaccine: Health Canada recommendations for people with serious allergies:
https://recalls-rappels.canada.ca/en/alert-recall/pfizer-biontech-covid-19-vaccine-health-canada-recommendations-people-serious - Government of BC > Get Your Booster Dose:
https://www2.gov.bc.ca/gov/content/covid-19/vaccine/booster - BCCDC > Children and COVID-19 Vaccination:
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/covid-19-vaccine/vaccines-children - Government of BC > Proof of Vaccination and the BC Vaccine Card:
https://www2.gov.bc.ca/gov/content/covid-19/vaccine/proof - Government of Canada > COVID-19: How to care at home for someone who has or may have been exposed:
https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/how-care-someone-covid-19-home.html - Government of Canada > Post COVID-19 Condition:
https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/symptoms/post-covid-19-condition.html - Government of Canada > Latest information on COVID-19 in federal correctional institutions:
https://www.canada.ca/en/correctional-service/campaigns/covid-19/latest-information.html - Government of BC > Provincial and regional restrictions:
https://www2.gov.bc.ca/gov/content/covid-19/info/restrictions - Government of Canada > Canada’s COVID-19 Economic Response Plan:
https://www.canada.ca/en/department-finance/economic-response-plan.html - Government of BC > Paid Sick Leave:
https://www.gov.bc.ca/PaidSickLeave - Government of BC > BC’s Restart Plan:
https://www2.gov.bc.ca/gov/content/covid-19/info/restart - BCCDC > How to Find Trusted Information About Vaccines:
http://www.bccdc.ca/health-info/diseases-conditions/covid-19/covid-19-vaccine/how-to-find-trusted-information-about-vaccines